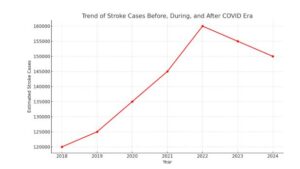
Strokes After COVID Era: In the years following the global COVID-19 pandemic, a concerning trend has emerged: an apparent increase in heart attacks and strokes. This rise has prompted a global discussion among medical experts, researchers, and public health organizations like the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC). While the full picture is still unfolding, credible sources and peer-reviewed journals are shedding light on possible connections between COVID-19 and these serious health events.
What Are We Seeing?
Across the globe, doctors and hospitals have reported seeing more cases of heart attacks and strokes, even in people who didn’t have a history of heart problems. This isn’t just a feeling; large-scale studies are showing a real increase.
Read More: University of Kalyani Recruitment 2025 | Apply Online for Sub-Assistant Engineer (Civil) Post
For example, a study published in a peer-reviewed journal found that people who had COVID-19 had a significantly higher risk of major heart and brain events (like heart attack or stroke) even up to three years after their initial infection. This risk was especially higher for those who had severe COVID-19 and needed to be hospitalized. Some research even suggests that COVID-19 could double the risk of these events.
Why Might This Be Happening?
Experts Point to Several Factors:
1. The Virus Itself Can Cause Direct Damage:
- Inflammation and Blood Clots: COVID-19 is known to cause widespread inflammation in the body. This inflammation can damage the lining of blood vessels, making them more prone to forming dangerous blood clots. If these clots block blood flow to the heart, it leads to a heart attack. If they block blood flow to the brain, it causes a stroke.
- Direct Heart and Artery Infection: Studies have found the SARS-CoV-2 virus (which causes COVID-19) in the walls of arteries and even within the heart muscle itself. This direct infection can trigger an inflammatory response, potentially destabilizing existing plaques (fatty deposits) in the arteries, making them more likely to rupture and cause a blockage.
- Myocarditis: This is an inflammation of the heart muscle, and it’s a known complication of COVID-19. Myocarditis can weaken the heart and lead to irregular heartbeats, increasing the risk of heart problems.
2. The Body’s Immune Response Plays a Role:
- “Cytokine Storm”: In some severe cases of COVID-19, the immune system overreacts, leading to a “cytokine storm.” This intense immune response can cause significant damage throughout the body, including the cardiovascular system.
- Long COVID and Persistent Inflammation: Many people experience “Long COVID” (also known as Post COVID-19 Condition), where symptoms linger for months after the initial infection. Research suggests that persistent inflammation in the heart and lungs can be a feature of Long COVID, even if standard tests appear normal. This ongoing inflammation could put individuals at a higher risk for future heart and lung issues.
3. Indirect Effects and Lifestyle Changes:
- Increased Stress and Anxiety: The pandemic brought immense stress, anxiety, and changes to daily routines for many. High stress levels can negatively impact heart health, potentially contributing to higher blood pressure and other risk factors.
- Delayed Medical Care: During the height of the pandemic, some people may have delayed seeking medical attention for non-COVID-related health concerns, including early signs of heart disease, due to fear of infection or overwhelmed healthcare systems. This could mean some conditions worsened before treatment.
- Changes in Lifestyle: Lockdowns and restrictions led to changes in diet, exercise habits, and increased sedentary behavior for many, all of which can contribute to heart disease risk.
What Do Major Health Organizations Say?
- WHO (World Health Organization): The WHO recognizes Long COVID as a significant health issue and is actively involved in research and guidance related to its effects, including cardiovascular complications. They emphasize the importance of understanding the long-term impacts of COVID-19.
- CDC (Centers for Disease Control and Prevention): The CDC has been tracking and reporting on the various health impacts of COVID-19, including its effects on the heart and brain. Their data aligns with findings that show an increased risk of cardiovascular events after COVID-19 infection. The CDC recommends vaccination to prevent severe COVID-19 and its complications.
What Can You Do?
While the research continues, here’s what experts recommend to protect your heart and brain health, especially if you’ve had COVID-19:
- Stay Vaccinated: COVID-19 vaccination is a key step in preventing severe illness, which is strongly linked to higher risks of heart attacks and strokes.
- Manage Existing Health Conditions: If you have conditions like high blood pressure, diabetes, or high cholesterol, it’s crucial to manage them carefully with your doctor.
- Adopt a Healthy Lifestyle:
- Eat a balanced diet rich in fruits, vegetables, and whole grains.
- Stay physically active with regular exercise, gradually increasing intensity if you’re recovering from COVID-19. Listen to your body and don’t overdo it.
- Quit smoking and limit alcohol intake.
- Get enough quality sleep.
- Manage stress through techniques like meditation, yoga, or hobbies.
- Listen to Your Body and Seek Medical Advice: If you experience any new or unusual symptoms, especially chest pain, shortness of breath, sudden weakness, or dizziness, don’t hesitate to seek medical attention. Early detection and treatment can make a big difference.
The Road Ahead of Strokes After COVID Era
The relationship between COVID-19 and the increased incidence of heart attacks and strokes is a complex area of ongoing research. What is clear is that COVID-19 is not just a respiratory illness; it can have lasting effects on the body, including the cardiovascular and neurological systems. By staying informed, following health guidelines, and prioritizing a healthy lifestyle, we can all work towards reducing these risks in the post-COVID era.

